MACRA Monday: Clinical Practice Improvement Performance Category

MACRA Monday: Clinical Practice Improvement Performance Category November 14, 2016
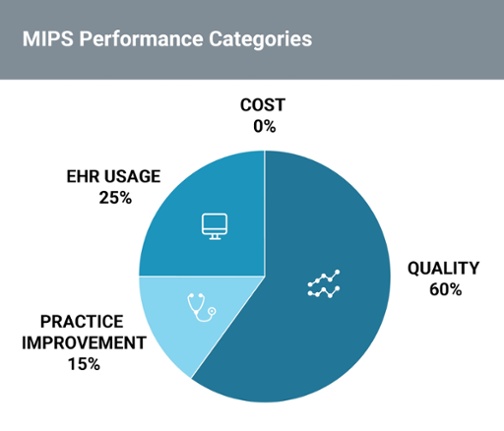
Every Monday this month, we’ll be breaking down the four performance categories that independent practices will be required to report on when the Merit-based Incentive Payment System or MIPS track of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) law goes into effect on January 1, and providing you with tips and strategies on how to succeed during this transition.
The Clinical Practice Improvement Activities (CPIA) performance category is a new reporting requirement introduced as part of the shift to quality-based reimbursements via MACRA. Unlike MACRA’s other performance categories, CPIA does not replace any previous programs and instead focuses on helping practices implement a “patient-centered approach to program development that leads to better, smarter, and healthier care,” according to the Centers for Medicare Medicaid Services (CMS).
What are the requirements?
As part of the requirements for this performance category, MACRA/MIPS participants are required to select one CPIA activity (out of 90+ proposed activities) to at minimum receive a partial score, with additional credit for multiple activities.
Subcategories of Clinical Practice Improvement Activities
| Expanded Practice Access | Beneficiary Engagement | Achieving Health Equity |
| Population Management | Patient Safety and Practice Assessment | Emergency Preparedness and Resposne |
| Care Coordination | Participation in an APM, including a medical home model | Integrated Behavioral and Mental Health |
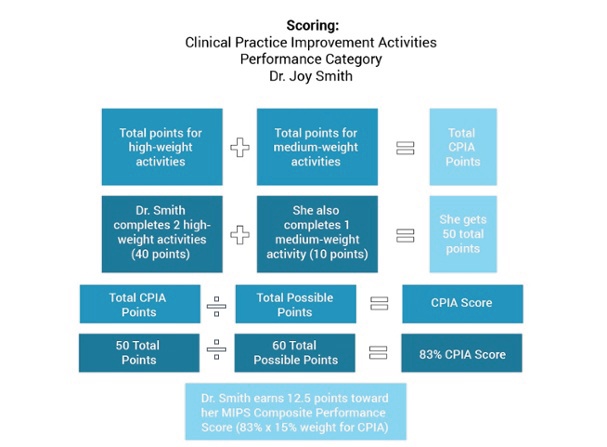
Furthermore, CPIA activities can be categorized as either “high” or “medium” weight, with providers earning 20 or 10 points each, respectively. In order for a participant to receive “full credit,” they must earn 60 points.
Clinical Practice Improvement Activities Examples:
- Expanded Practice Access: expanding access to services, extending practices hours and telehealth access
- Population Management: participation in programs that track population outcomes such as chronic care management programs
- Care Coordination: participation in various CMS models that improve care coordination, improvement of care coordination processes
-
Beneficiary Engagement: use of EHRs to document patient-reported outcomes, use of patient portals and patient engagement tools
-
Patient Safety and Practice Assessment: regular practice assessments and patient safety improvements
How are Clinical Practice Improvement Activities calculated?
Scores for this performance category can be calculated by simply combining points for both high-weight categories and medium-weight categories and dividing by the 60 possible points to receive a percentage score that can then be translated into points based on CPIA’s weight as a performance category. A primary care provider in a solo practice, like the one in the example provided below, might calculate their score like this:
Key Takeaways:
- The Clinical Practice Improvement Activities is an entirely new performance category that unlike other performance categories does not replace a previous program.
- This category aims to improve clinical practice or care delivery in an effort to improve outcomes and reward quality over quantity.
- Participants have over 90 options for how they’d like to receive points that are totaled and weighted as either high-weight or medium-weight.
Subscribe to our MACRA Resource Series to recieve content like this straight to your inbox!
![]()






