How Elation ensures that MIPS providers avoid penalty

How Elation ensures that MIPS providers avoid penalty November 16, 2017
As the first year of the Merit-based Incentive Payment System (MIPS) track for MACRA comes to a close, many physicians participating in the program might be wondering what action they need to take to avoid costly penalties. With Elation’s built-in dashboards and health policy support, you can put your stresses at ease and avoid penalties in 2019, as a result of performance in 2017.
How do you report for MIPS in 2017?
The Centers for Medicare & Medicaid Services (CMS) recently loosened some of the requirements of the program. These requirements mean 2017 is a transition year for MIPS and the minimum practices need to do is report some data to test the program and avoid penalties.
MIPS providers can choose to report either:
- 1 Quality Measure OR
- 4 Advancing Care Information Base Measures OR
- 1 Improvement Activity
How can you keep track of your performance through Elation?
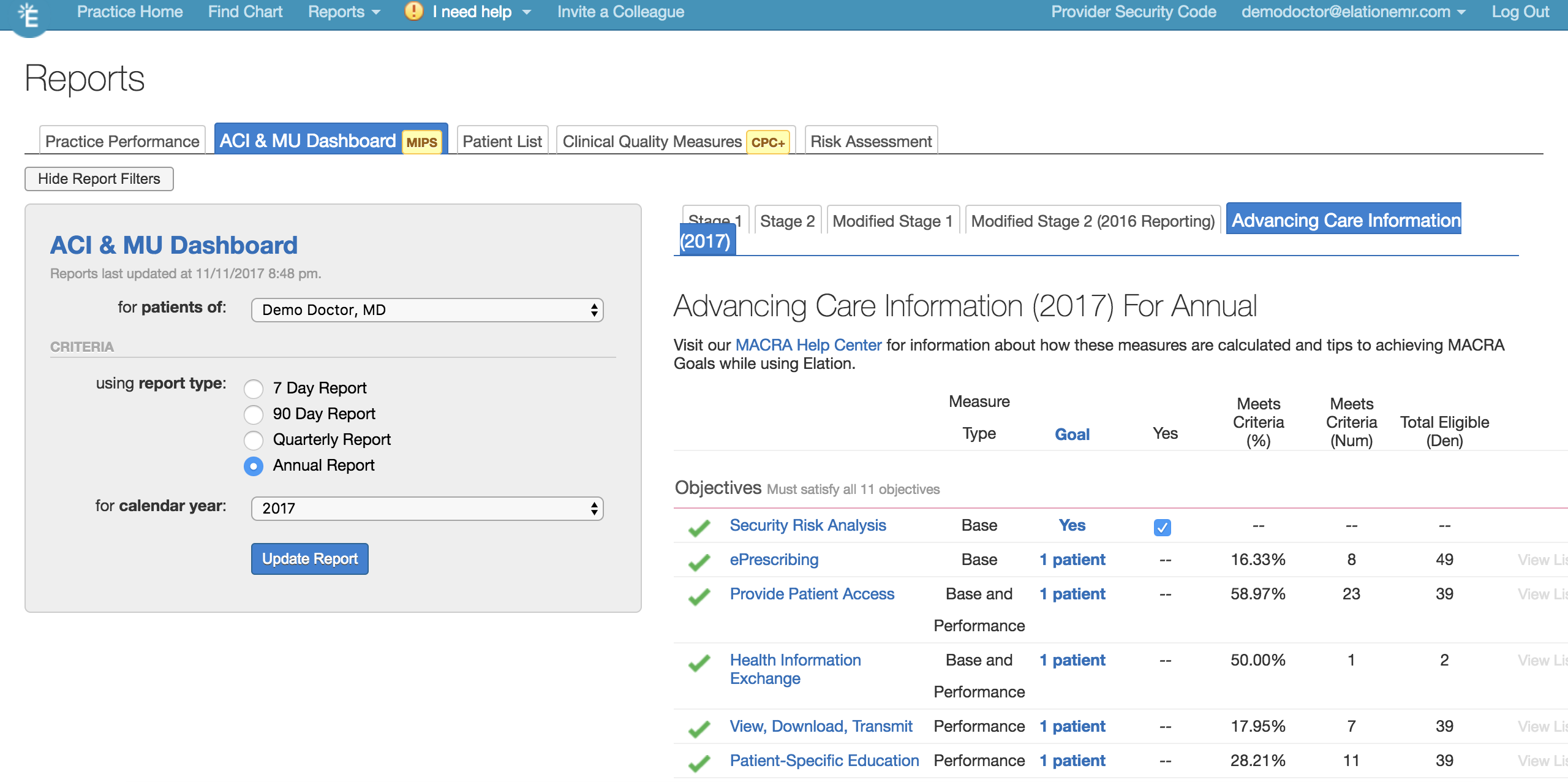
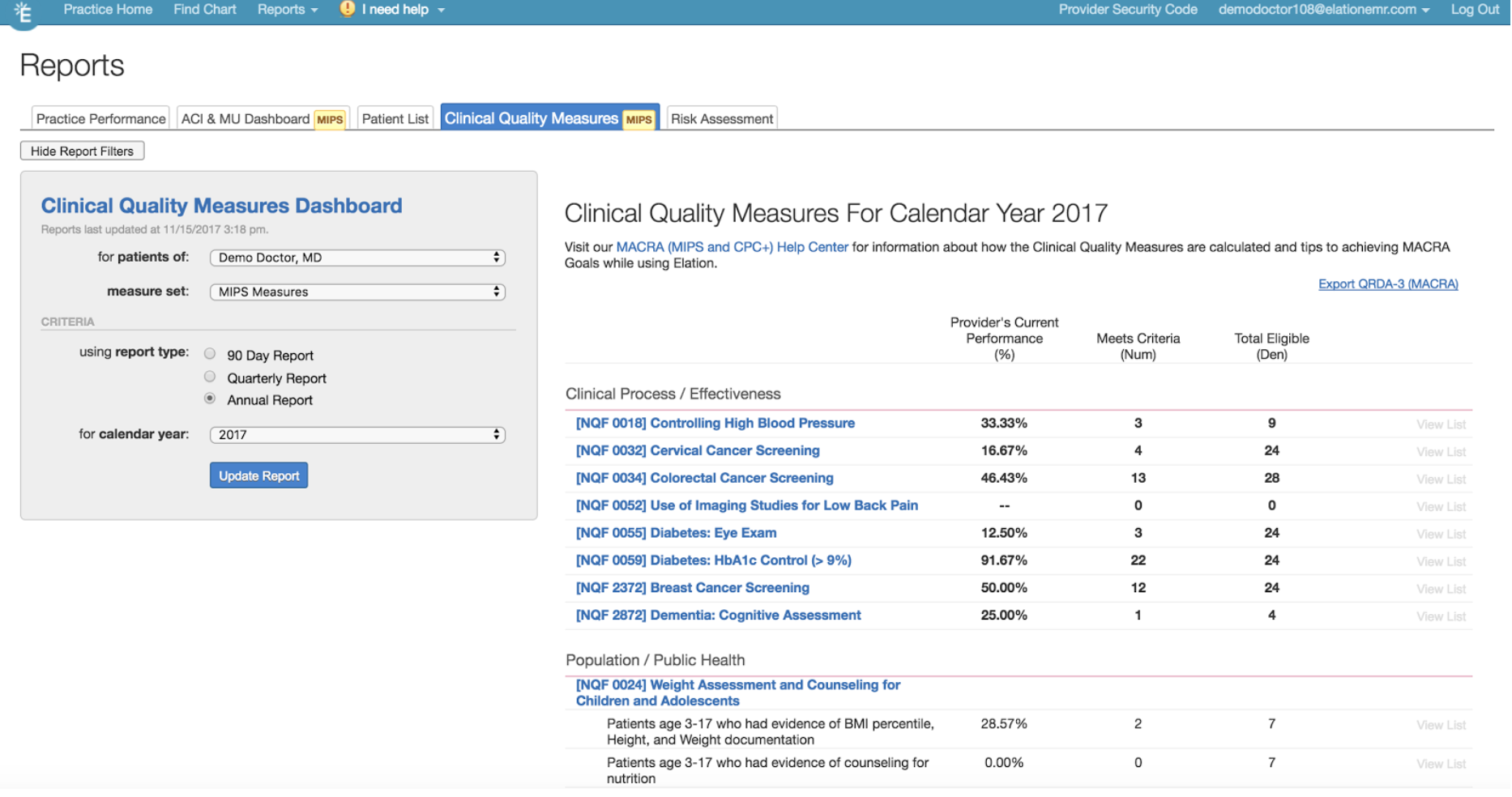
Within Elation’s “Reports” section, practices can access the ACl and CQM dashboards.
In the ACI dashboard, you can view progress on the four base measures.
The CQM dashboard shows clinical performance on quality measures and provides access to a patient list where you can address some of these measures.
With these useful features, providers can spend less time worrying about quality programs and spend more time providing quality care to their patients. Elation is here for you and your practice during the transition to value-based care. For a more detailed overview on MIPS, watch this webinar below:






