Policy update: MACRA implementation and the move to Value-Based Care
Policy update: MACRA implementation and the move to Value-Based Care May 3, 2016
Last week, the Department of Health and Human Services (HHS) issued a long-awaited proposal to revamp how Medicare pays physicians and other clinicians for quality. This Notice of Proposed Rulemaking is the first step in implementing the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).
|
“We’re proposing today to replace meaningful use in the physician office with a new effort that moves the emphasis away from the use of information technology to one that support patient care supported by better and more connected technology,” explains CMS Acting Administrator Andy Slavitt. |
These new rules come in response to their announcement this past January for plans to phase out the Meaningful Use quality reporting program for Medicare physicians — a welcome change for many US providers, who have collectively spent more than $15.4 billion a year1 dealing with the reporting of quality measures.
This move to standardize measures will introduce the new Quality Payment Program (QPP), a value-based reimbursement model that aims to improve outcomes through two main arms: the Merit-Based Incentive Payment System (MIPS) and the Advanced Alternative Payment Models (APM).
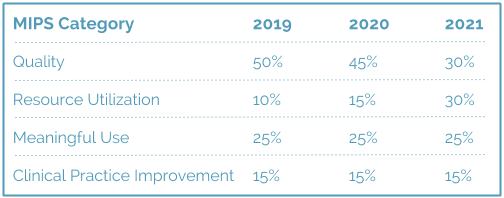
CMS has reported that these new payment models should give healthcare providers more flexibility with quality reporting, and are designed to consolidate the current Meaningful Use, Physician Quality Reporting System, and Value-based Payment Modifier programs. Payments under MIPS, for example, will take into account a sliding scale of measures tied to quality, resource utilization, meaningful use of an EMR, and clinical practice improvement.

Additional resources have since become available from the American Medical Association (AMA) who have recently released eight educational modules as part of the STEPS Forward program, to help providers better understand the specifics of MACRA implementation and the overall move to pay-for-value care models.
The proposal, if finalized, would kick off reporting as of January 1, 2017. In the interim, we will continue to monitor the industry for any new changes and will make sure that you are consistently kept up to date as the policy evolves.






