93% of MIPs-eligible providers will receive a positive payment adjustment

In a blog post published on November 8, 2018, Seema Verma, Administrator for the Centers for Medicare & Medicaid Services (CMS), shared data on the Quality Payment Program (QPP) Year 1 Performance. The results were overwhelming positive, with 93 percent of MIPS eligible clinicians receiving a positive payment adjustment for their performance in 2017 and 95 percent overall avoiding a negative payment adjustment.
CMS calculated that “1,057,824 MIPS eligible clinicians will receive a MIPS payment adjustment, either positive, neutral, or negative. Of that population, 1,006,319 MIPS eligible clinicians reported data as either an individual, as a part of a group, or through an Alternative Payment Model (APM) and received a neutral payment adjustment or better. Additionally, under the Advanced APM track, 99,076 eligible clinicians earned Qualifying APM Participant (QP) status.”
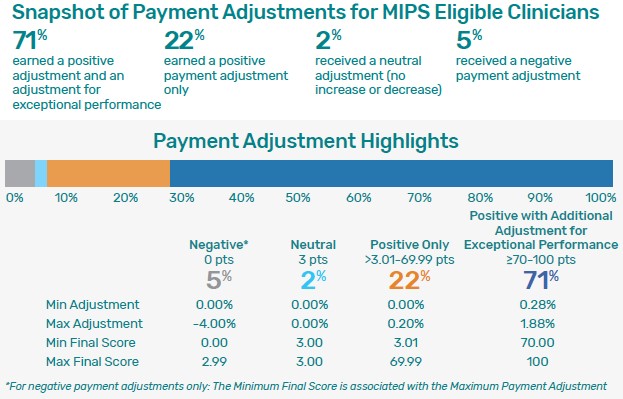
In her blog post, Verma provided a chart that illustrates the numbers for the various payment adjustments:
CMS recognizes that even though the majority of providers received a positive payment adjustment, those adjustments were “modest.” MIPS has a budget neutrality requirement, established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). In addition, during the transition year of 2017, CMS offered providers a relatively low overall performance threshold for MIPS as well as a “pick your pace” option that provides three reporting options of test, partial year, or full year. These accommodations were offered to encourage flexibility and more robust provider participation.
Verma emphasized that, going forward, CMS is “committed to continue leveraging our Patients over Paperwork framework to review many of the MIPS requirements to reduce burden and add additional flexibilities so clinicians can successfully participate without sacrificing the time they spend with patients.” Providers are encouraged to send CMS feedback to “help identify areas of immediate need as well as shape the program for future performance years.”






