How COVID-19 is affecting independent primary care

Life is moving fast for independent primary care practices. While still struggling during COVID-19, thankfully, there is new support and signs of adaptation. Here’s what we’re seeing at Elation Health for our 14,000 primary care and direct primary care clinicians and their 7 million patients.
First, here’s the good news. We are grateful that 3 new relief plans will help our practices stay afloat and caring for their patients: 1) A policy change for video and phone visits 2) CMS is advancing 3 months of Medicare payments 3) SBA loans to help medical practices cover payroll and rent.
ATTN: big news from @CMSGov tonight – physicians will now be able to bill for care provided via telephone only. Important policy change. Thank you to @SeemaCMS and her team for this important change in payment policy. Big for @aafp members. pic.twitter.com/vbyMwPWYOx
— Shawn Martin (@rshawnm) March 30, 2020
This is a step in the right direction, but independent practices are still struggling significantly. The increased reimbursement for phone visits we want to see hasn’t happened yet. Terrific reporting by Christina Farr on the practice emergency last week:
Because most of U.S. health care is fee for service, scaling back elective procedures could lead to cuts of medical personnel at a time when we need them the most:
“I’ve heard some stories of doctors using their own savings to pay staff” – @DaniaPal https://t.co/3E1GvSPeSk
— Christina Farr (@chrissyfarr) March 31, 2020
Last week we saw another 5% WoW increase in cancellations, to add on top of the 48% increase experienced last week. Overall we’re seeing almost 40% of appointments being canceled.

Some patient encounters are shifting to phone and video calls, but overall, independent primary care practices are facing another week of a 30% decrease in their total patient volume.
Patient phone calls are still far above normal, but starting to decrease from the high two weeks ago. One practice says “It’s very difficult to keep up with all the phone calls while seeing many patients ‘curbside’ outside of the office in their own cars when they are ill.”
This is not what we expected. The biggest increase in phone calls to primary care practices is coming from patients in the 40-69 year old demographic. There was a 35% spike in calls from those patients just last week.
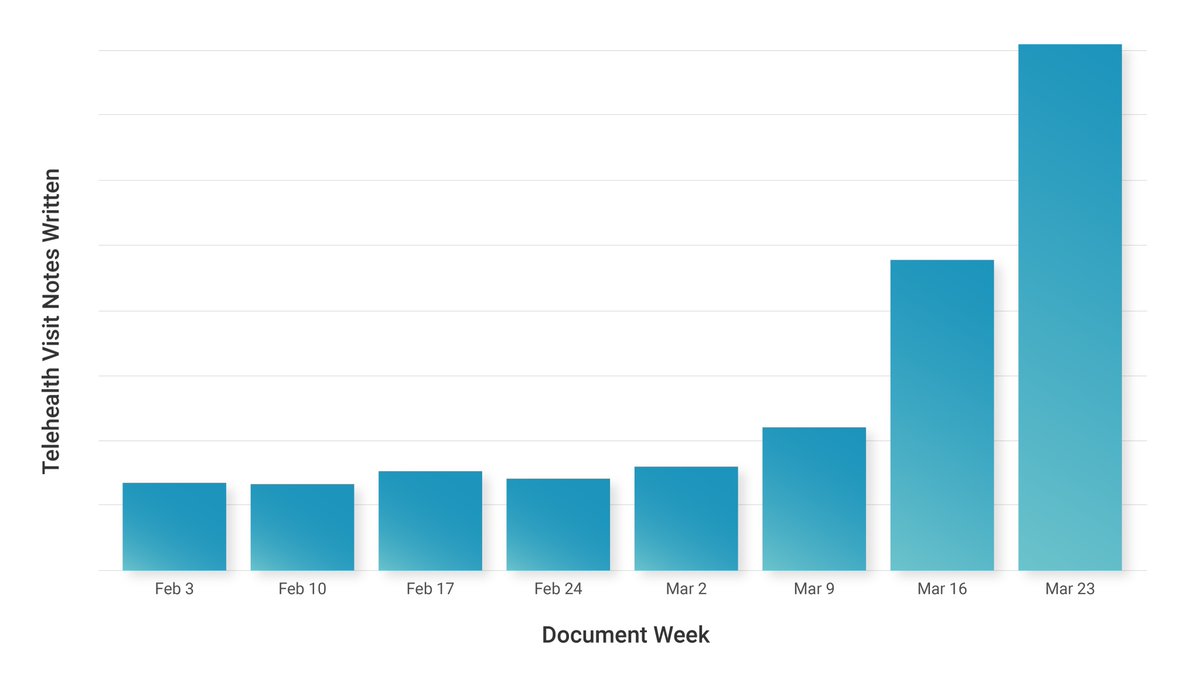
Our hunch is that the decrease in phone call visits is because practices so quickly adopted telemedicine to get a more normal reimbursement. 41% of our practices had never used telehealth before COVID 19 and we’re doing a ton of support for the transition.
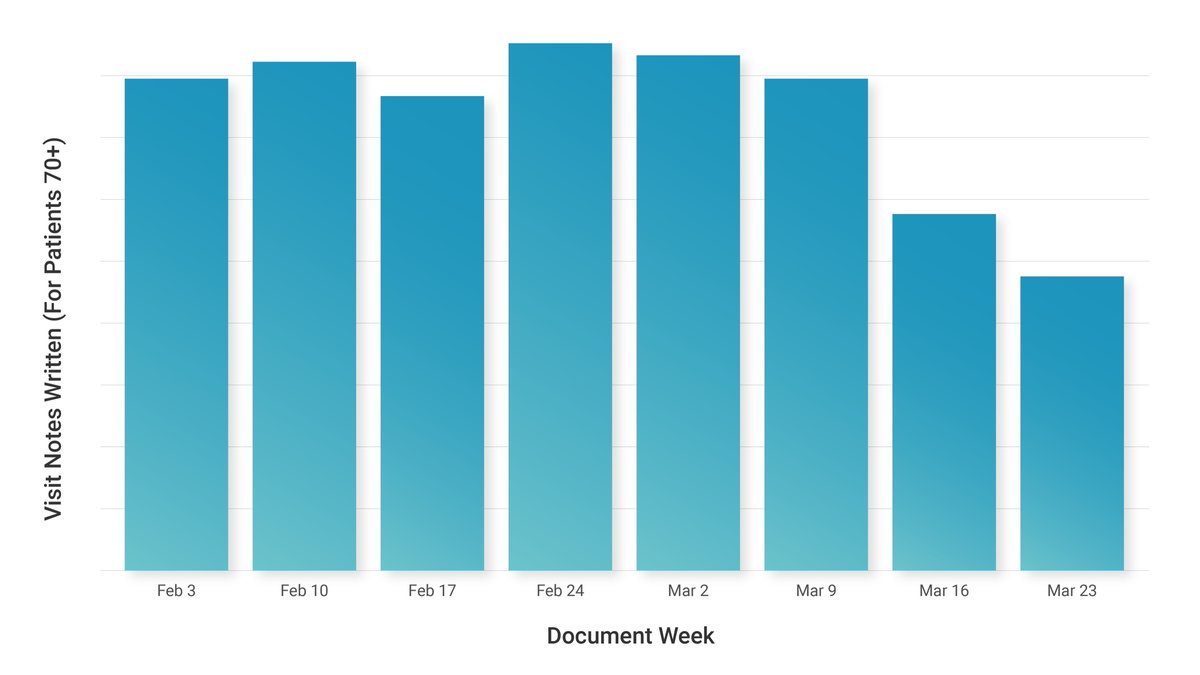
A worrisome trend we’re watching is patients over 70 years old are receiving a lot less primary care in any format. We’ve seen a more than 50% decrease in interactions with these older patients compared to normal.
There are mixed reports from the frontlines: “We can do many things remotely so staffing isn’t an issue. Our employees are safe with us!”, “Only a few N95 masks left”, “We are down to a skeleton staff right now. We never have enough help to begin with so it’s very difficult.”
Thankful for the voices of Shawn Martin, AAFP, and Dr. Farzad Mostashari who are continuing to raise the alarm and advocate for our docs on the frontlines. Stories like this in the LA Times helped a lot to alert people to the dangers practices are facing.
What else would you like to know about what’s happening with independent primary care in the US? We’re happy to share the latest about this crucial segment of our healthcare system.






