Electronic Prior Authorization: Reducing the Burden in Primary Care with Elation
For decades, prior authorization has been one of the biggest administrative bottlenecks in healthcare. Historically, physicians themselves were forced to complete the process—spending hours on phone calls and faxes instead of with patients.
The burden is measurable: physicians spend $2,161 to $3,430 annually per doctor just to manage prior authorizations, along with hours of staff and clinician time every week. Yet, the vast majority of these requests are approved. In fact, Kaiser Family Foundation reports that Medicare Advantage insurers processed nearly 50 million prior authorization requests in 2023, and 97% were approved.
That means countless hours are wasted chasing approvals that nearly always go through—a system that drains resources without meaningful impact on care.
Why Prior Authorization Persists
Payers argue that prior authorization ensures cost-effective, evidence-based care. But for primary care clinicians, prior authorization rarely prevents unnecessary treatments. Instead, it creates delays in care delivery, burdens already stretched teams, and erodes patient trust when approvals take too long.
As one of the most common friction points in healthcare, prior authorization has become a symbol of administrative inefficiency—one that urgently needs modern solutions.
Enter Electronic Prior Authorization (ePA)
Electronic prior authorization, or ePA, transforms this outdated process by bringing approvals online. Instead of faxing paperwork or waiting on hold with payers, clinicians can submit and track requests digitally, often in real time.
Studies show that ePA reduces turnaround time, lowers the need for manual follow-up, and helps practices complete routine approvals more efficiently. While it doesn’t eliminate the requirement itself, it makes the experience far less disruptive to care delivery.
How Elation Simplifies ePA for Primary Care
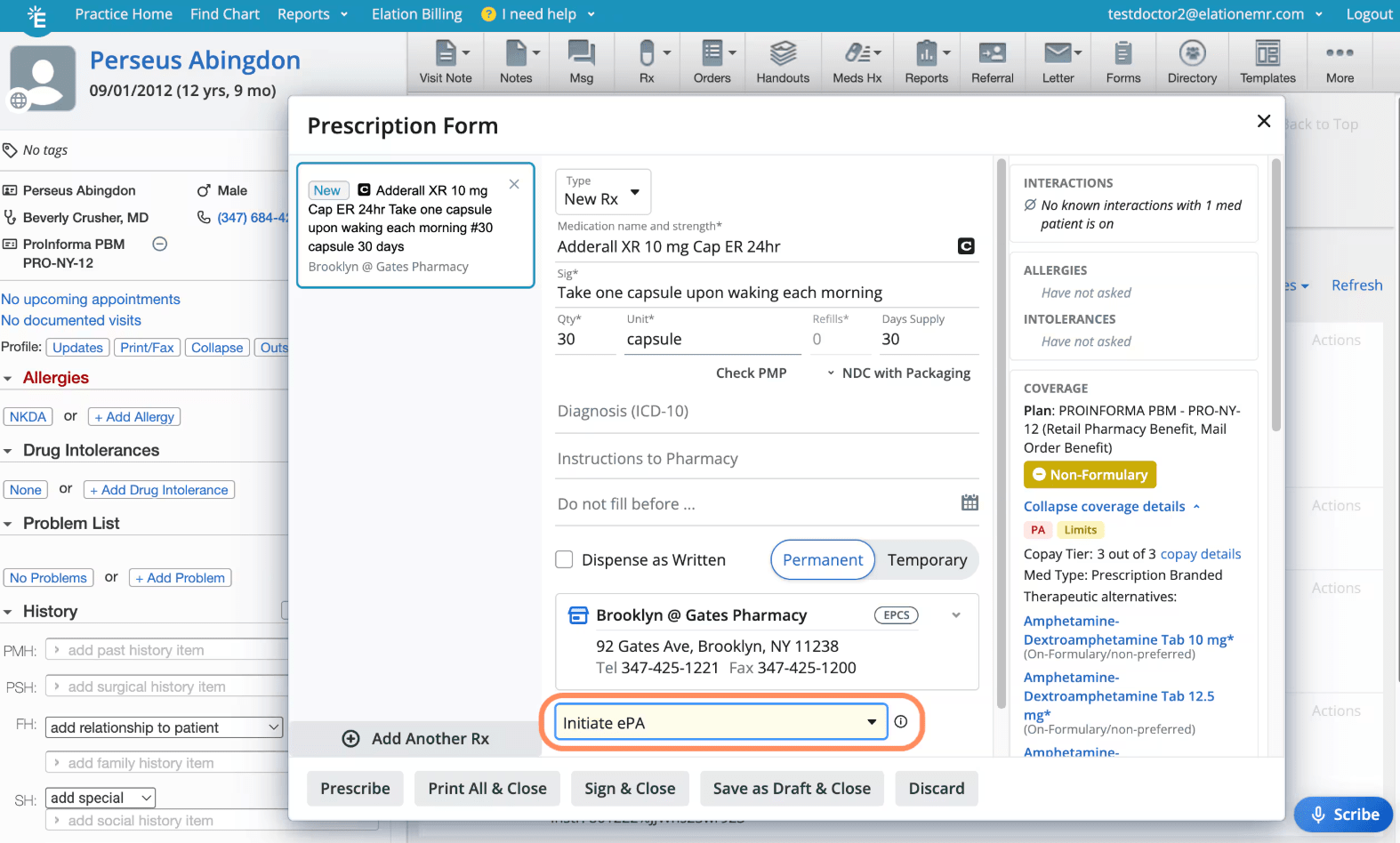
Elation has embedded ePA directly into its EHR workflow, so prior authorization can be handled where it belongs—inside the patient chart. With Elation, practices can:
-
Initiate and submit requests directly from the EHR without duplicate data entry.
-
Track authorization status in real time, avoiding the frustration of chasing updates.
-
Attach supporting documentation seamlessly from within Elation.
-
Receive automated notifications when an authorization is completed, reducing manual checks.
By eliminating payer portals and paper forms, Elation turns prior authorization into a task that doesn’t derail the day. The result: less administrative burden for staff and faster access to care for patients.
Policy Momentum Is Building
The healthcare system is also recognizing the inefficiency of prior authorization. Insurers like Humana have pledged to reduce PA requirements starting in 2026. A bipartisan bill—the Improving Seniors’ Timely Access to Care Act —calls for mandatory ePA adoption in Medicare Advantage by 2027. Meanwhile, CMS rules now require faster responses, with payers obligated to reply within 7 days for routine requests and 72 hours for urgent ones.
These reforms signal that ePA is not just an option but the future standard for prior authorization.
The Path Forward
Prior authorization isn’t going away—but with electronic tools, it no longer has to be a roadblock. For primary care practices, the shift to ePA means fewer bottlenecks, less wasted time, and more time spent with patients.
At Elation, our mission is to empower primary care with tools that relieve cognitive burden, reduce administrative drag, and support high-quality care. Our integrated ePA solution is one more way we help practices focus on what matters most—patients, not paperwork.
Ready to Streamline Prior Authorization?
Discover how Elation can simplify prior authorization for your practice. Request a demo today and see how ePA can save time, reduce frustration, and help your team focus on delivering exceptional patient care.
