Making Sense of MIPS: What it Means for Primary Care
Making Sense of MIPS: What it Means for Primary Care February 5, 2016
In April of last year, Congress made major changes to the reimbursement system for Medicare and Medicaid patients.
What does this mean for primary care physicians and their practices? Yesterday, the American Academy of Family Physicians made a great post detailing how doctors can expect to be affected by the changes.
What the AAFP’s article says:
-
A Merit-Based Incentive Payment System (MIPS) will be introduced in 2019 to replace the current Physician Quality Reporting System (PQRS), Meaningful Use (MU), and Value-Based Modifiers (VBM) programs.
-
The new system will focus on giving a single score on a per-physician basis.
-
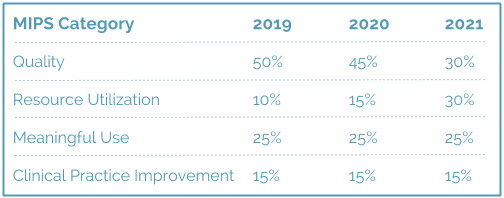
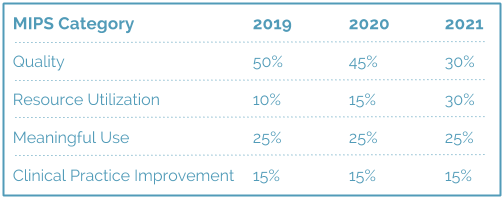
This score will be calculated using the following criteria:
-
There is potential that MIPS will employ a two-year lookback, meaning 2017 would be the starting year for physicians to qualify under the new criteria.
-
MIPS is a specific track of payment for the Medicare Access & CHIP Reauthorization Act of 2015 (MACRA), the sole source of Medicare reimbursement.
What this means for independent physicians and their practices:
-
Adopt Technology: Meaningful use of an electronic health record will continue to be important for primary care practices who earn significant revenue from Medicare reimbursements.
-
Report Accurately: Your practice will need to shift how you report your use of EMR to the government, or you’ll see a dip in Medicare payments coming in.
-
Focus on Outcomes, not Service Delivery: Measuring the quality of your care and patient outcomes will become increasingly important revenue drivers for your practice, and use of your electronic health record system should support this.
-
Act Fast: Be ready – while the table above shows a 2019 start, CMS has traditionally used a two-year look back period, so starting in 2017 you should be ready to comply.






